A concise review on the complex interaction between the brain and the skin, and how our state of mind could provoke the occurrence of skin disorders.
More than 30% of of every dermatological disorders are influenced by psychological factors. These conditions are referred to as psychodermatological disorders, which are further classified into four categories further explained below.
types of psychodermatological disorders
Physiopsychological dermatoses
- Skin diseases that are precipitated or aggravated by psychological stress.
- Examples: Psoriasis, acne vulgaris, atopic dermatitis, urticaria, etc
Psychopathology focused on the skin
- As seen in self-inflicted diseases and diseases in which skin lesions are not present.
- Examples: Dermatitis artefacta, trichotillomania, body dysmorphic disorder, delusions of parasitosis, etc.
Dermatoses with psychiatric manifestations
- Emotional problems that arise due to the existence of skin disorders.
- Examples: Anxiety caused by acne, albinism, ichtyoses, vitiligo, alopecia, etc.
Cutaneous disorders
- Unpleasant sensationson the skin, such as itching and dysesthesia.
- Examples: Psychogenic itch, vulvodynia, etc.
HOW DOES STRESS AFFECT THE SKIN?

EXAMPLES OF PHYSIOPSYCHOLOGICAL DISORDERS
Acne Vulgaris
- Increased acne severity is significantly associated with stress levels
- Promotion of sebum production, infundibular keratinocyte differentiation, and induction of cytokines lead to inflammation
- The rise of substance P nerve fibers in acne supports the proliferation of sebaceous glands
Atopic Dermatitis
- Hyporesponsive HPA axis enhances the chronic Th2-predominant immune response
- Pathological behavior such as itching, scratching, and poor self-care may accelerate disease progression
- Interestingly, chronic stress in the early years of life (history of abuse, babies born from depressed mothers) may increase vulnerability to AD by persistent sensitization of the HPA axis
Psoriasis
- Stress is a trigger in 33-80% cases
- Proinflammatory cytokines expressed in psoriasis (IL-1, IL-6, and TNF-a) activate mast cells and trigger a disruption in the proliferation and differentiation of keratinocytes
- Women, younger patients, early onset, and those with lesions in areas not covered by clothing are more susceptible to disease initiation and progression
Skin tumors
- Cellular immune responses under acute stress may have tumor-preventive effects
- On the other hand, under chronic stress, a weakened cellular immune response accompanied with the rise in regulatory T cells are tumor-permissive
- CRH, ACTH, and a-MSH peptides are highly expressed in malignant tumors compared to normal skin
THE RIGHT APPROACH TO PSYCHODERMATOSES
Despite their relevance, psychosocial aspects of diseases are rarely addressed by doctors and patients. So, how do we, as physicians, properly treat this condition?
History taking
- History taking should include psychosocial factors and their interaction to the development of skin diseases:
- When and where the did the lesions first appear? What was the situation like and how did the patient react?
- Were there flare-ups, and were they preceded by stressful events?
- Derivation of potential interaction
- Do these events coincide with the course of disease?
- What psychological consequences do the patient bear due to this diagnosis?
- Which measures are taken by the patient and are they helpful?
Attitude
Let the patient address their symptoms in their own words. If possible, engage in a discussion with the patient about their symptoms. Remember, the consultation itself signifies stress. Hence, be neutral, non-judgmental, and open.
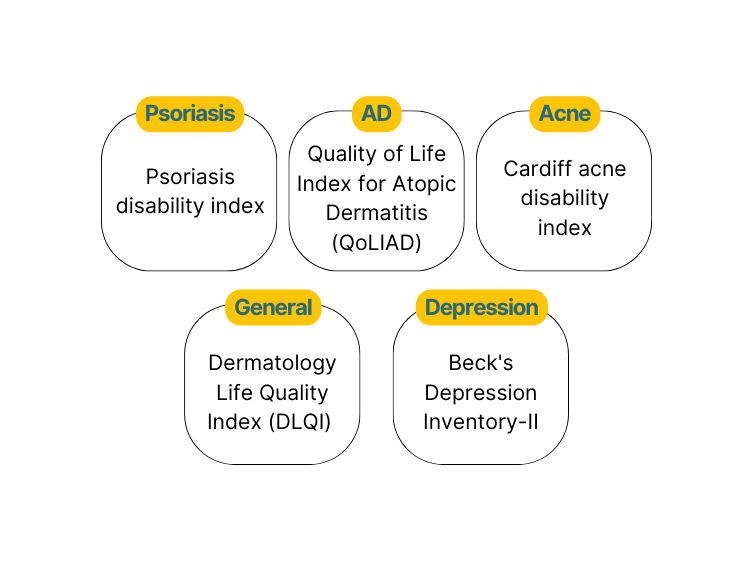
Diagnostic measures
Several self-assessment questionnaires addressing mental health and distress can be utilized to document triggers and assess the effectivity of therapy.
When to refer?
Ideally, management of all psychodermatology disorders require psychotherapy and psychotropics. Hence, patients with severe psychiatric manifestations should be immediately referred to a psychiatrist.
REFERENCES
- Chen Y, Lyga J. Brain-Skin Connection: Stress, Inflammation and Skin Aging. Inflamm Allergy Drug Targets. 2014;13(3):177-190.
- Evers A, van Beugen S. How stress affects the skin: from designs to mechanisms. Br J Dermatol. 2021;185(1):12-13.
- Jafferany M, Ferreira B, Abdelmaksoud A, Mkhoyan R. Management of psychocutaneous disorders: A practical approach for dermatologists. Dermatol Ther. 2020;33(6).
- Jafferany M, Ferreira B, Patel A. The Essentials of Psychodermatology. Switzerland AG: Springer International Publishing; 2020:29-34.
- Peters E. Stressed skin? – a molecular psychosomatic update on stress-causes and effects in dermatologic diseases. JDDG – J Dtsch Dermatol Ges. 2016;14(3):233-252.
- Kim J, Cho B, Cho D, Park H. Expression of Hypothalamic–Pituitary–Adrenal Axis in Common Skin Diseases: Evidence of its Association with Stress-related Disease Activity. Acta Dermatol Venereol. 2013;93(4):387-393.